Table of Content
No fee schedules, basic unit, relative values or related listings are included in CDT-4. The ADA does not directly or indirectly practice medicine or dispense dental services. The sole responsibility for the software, including any CDT-4 and other content contained therein, is with or the CMS; and no endorsement by the ADA is intended or implied. The ADA expressly disclaims responsibility for any consequences or liability attributable to or related to any use, non-use, or interpretation of information contained or not contained in this file/product. This Agreement will terminate upon notice to you if you violate the terms of this Agreement.
Adequate staffing is at a premium where demand is high but capacity remains low. Finding the “best practices” to achieve great outcomes with the right number of visits has continued to be the holy grail. It seems somewhat unfair given at the same time CMS is expanding the HHVBP program nationally where CMS expects to save the Medicare program $3.38 billion over the next five years. This COLA appears very low given the higher price and wage inflation we have seen over the last couple of years. Salaries have also been steadily increasing to counter the staffing shortages due to COVID and the “great resignation”. Section 210 of the MACRA extended the rural add-on, which is an increase of 3 percent of the payment amount otherwise made for home health services furnished in a rural area, to episodes and visits ending before January 1, 2018.
Health
Christian’s work as a Medicare expert has appeared in several top-tier and trade news outlets including Forbes, MarketWatch, WebMD and Yahoo! Finance. Join our email series to receive your free Medicare guide and the latest information about Medicare and Medicare Advantage. A .gov website belongs to an official government organization in the United States.
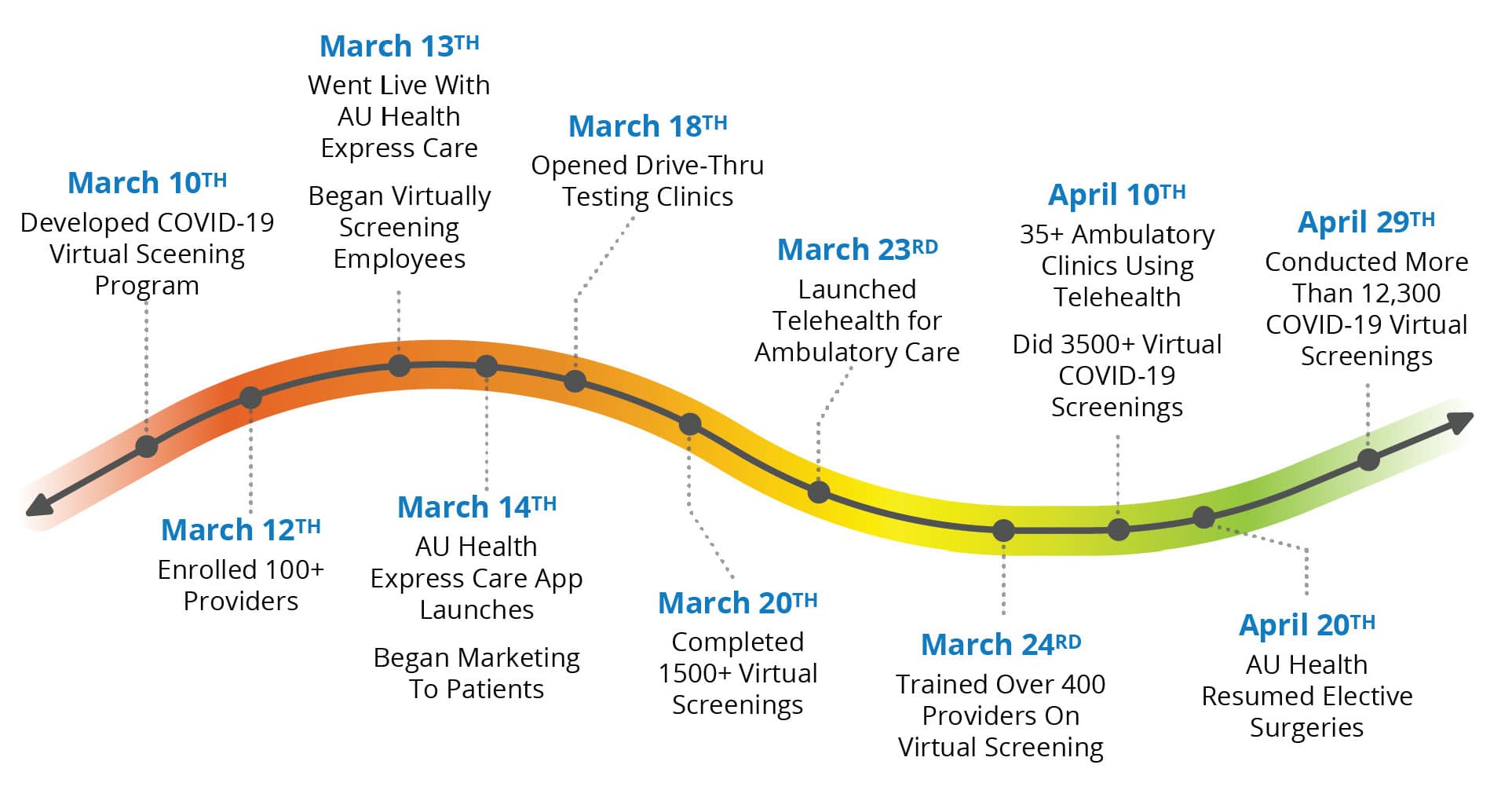
Some healthcare organizations have been wary of hospital-at-home programs without the guarantee of future Medicare reimbursement, and private insurers have been reluctant to reimburse that care due to a lack of outcome data. Some nurses and advocacy groups have questioned the safety of relying on remote technology in acute cases. The proposal extends the Centers for Medicare & Medicaid Services' hospital-at-home waiver through 2024. That waiver, established in November 2020 to increase capacity to accommodate COVID-19 patients, allow hospitals to handle emergency and inpatient cases outside of a facility. Hospitals nationwide embraced hospital-at-home programs as part of a larger push for virtual care options.
Ivy Rehab Network Physical Therapy and Rehab Professionals
CMS this month proposed establishing special enrollment periods for people who lose Medicaid or CHIP benefits because their income rose during the pandemic. States had expected to resume eligibility checks once President Joe Biden’s administration declared an end to the COVID-19 public health emergency. An estimated 18 million individuals could lose coverage when states start reviewing patients’ eligibility for Medicaid and the Children's Health Insurance Program, according to a December report from the Robert Wood Johnson Foundation. Local officials promised to pause trimming their public benefit rolls during the emergency declaration period in exchange for federal COVID-19 relief.

According to the report, home health agencies received an average of $93.93 per home health visit in 2015, an increase of $1.24 from 2014. In states that paid registered nurses or home health aides directly the average rate per visit was $87.26. In states that mandated reimbursement rates, the average rate per visit was $52.19. For the personal care services state plan option, the average rate paid to provider agencies was $18.82 per hour in 2015, a slight increase from $18.73 per hour in 2014. In states where personal care services providers were paid directly by the state or where reimbursement rates were determined by the state, the average reimbursement rate was $13.43 per hour in 2015.
Signup for email updates
The HCPCS code will also typically appear on your bill from the health care provider. Usually, a home health care agency coordinates the services your doctor orders for you. The proposal also would establish federal standards around provider directories for private Medicaid carriers and other managed care companies. Provider directory requirements are currently regulated by a patchwork of state laws.
Yesterday I showed you how much it cost for us to become approved for adoption in Ontario, Canada. Today Im discussing the pay and reimbursements we received as Foster Care/Kinship Care parents. NADAC rates are used to reimburse pharmacies for covered outpatient drugs, excluding clotting factor drugs, and Myers and Stauffer is the contractor responsible for maintaining the NADAC rates. You may be eligible for Medicaid coverage if you are an HHA in New York State and meet the eligibility requirements.
The funds’ sources of Medicare include payroll taxes and Medicare payments such as premiums, deductibles, copays, and coinsurances. The State reimburses doctors, hospitals, and insurance companies from this trust. Original Medicare has Part A and Part B, and the company pays 80% of the total costs after you meet the deductibles. Part C includes Medicare Advantage plans which unify and often include prescription medication coverage . The funds sources of Medicare include payroll taxes and Medicare payments such as premiums, deductibles, copays, and coinsurances. Part C includes Medicare advantage plans which unify and often include prescription medication coverage .

Also, providers are moving towards value-based approaches on the patient and quality of care. The CMS proposed rate cut may be revised based on industry comments and an updated cost-of-living factor before the final rule is promulgated. Given the likelihood of a significant behavioral adjustment, and future retroactive cuts from CY 2020 and CY 2021, now is the time to revisit the tools and strategies your agency utilizes to become more efficient. Pursuing quality outcomes to achieve higher star ratings and HHVBP scores will be essential, but hopefully at the “best practice” number of visits. Section 411 of the Medicare Access and Children’s Health Insurance Program Reauthorization Act of requires the market basket percentage increase to be one percent for home health payments for CY 2018.
The bill provides funding to boost marketing and outreach efforts for the nation’s new three-digit mental health hotline, 988. It transitions other mental health hotlines, including one for veterans, to the national network. The bill would also extend telehealth services through 2024 for federally qualified health clinics and rural health clinics. Some services may be entirely excluded from the limited benefits plan, while others may be prioritized, depending on the situation’s specifics. Please note that unlike AAC and NADAC rates, providers cannot appeal CFMAC rates or submit rate inquiries.
The agency had initially floated a 4.2% aggregate decrease in 2023, which would have marked one of the steepest home health Medicare cuts in years. Nonetheless, CMS is still phasing in other cuts and permanent adjustments related to the rebalancing of the Patient-Driven Groupings Model . Medicare is a state-regulated program for individuals aging 65+ or with a disability.
Once you meet the eligibility criteria, you can get Medicare, regardless of your income level. On the other hand, Medicaid is a state and joint federal program providing health insurance to low-income families. To implement the model though, CMS had to make assumptions about behavioral changes because of the new unit of Medicare payment. The agency finalized three behavioral assumptions around clinical group coding, comorbidity coding, and the Low Utilization Payment Adjustment threshold.

However, exceptions exist in the case of treatment from a non-participating provider or foreign treatment. More than half of Medicaid spending is attributable to the fee-for-service payment model, as determined by the Medicaid and CHIP Payment and Access Commission . Effective April 1, 2022, CFMAC rates will be used to reimburse pharmacies for clotting factor drugs when a clotting factor drug does not possess an Average Acquisition Cost rate. This rate is determined based on available acquisition cost data and publicly available data unique to each clotting factor drug.
Patient advocates worried that states rushing to remove individuals from public benefits would lead to people being mistakenly dropped from Medicaid and without time to enroll in new coverage. Although the Medicaid reimbursement rates are low, they vary according to State. Since the payment is low, physicians are reluctant to participate in a Medicaid program. AHA asked CMS to clarify in the final rule how the agency will account for the increased costs that are not reflected in the market basket update and how it will ensure patients maintain access to home health services.


No comments:
Post a Comment